You’re expecting, and suddenly, the terms “natural birth,” “lotus birth,” “home birth” start cropping up. It turns out there are more types of birth than you ever imagined! Got confused wondering what are the differences, the pros and cons? Let’s delve into it!

It seems like the old talk of “normal or cesarean” is a thing of the past. You get pregnant, and now there are so many birth options that you might even ponder if this baby can make an entrance from somewhere other than the routes we already know… Routes – that’s the key word that changes everything!
Routes of Birth
Regardless of whether you’ve heard about 80 or 8 types of delivery, the birth routes essentially boil down to two: either the baby arrives through surgery in the abdominal region (c-section) or via the vaginal route. In other words, birth routes aren’t equivalent to types of childbirth.
So, you might be wondering why there are so many “types of childbirth,” right? It’s because these types aren’t about where the baby will come out, but rather about how and in which place the baby comes into the world. It’s more about assistance, reception, care, ambience, and those details surrounding birth when we read about “types of childbirth.”
What are the different Types of Birth?
Commonly, there’s a reference to 8 types of birth (though some mention 9 types, including squatting birth, which I consider just a position, so I’m not including it here):
Cesarean Birth or C-Section
Cesarean birth is the surgical route recommended when a vaginal delivery is not advisable (e.g., due to fetal position as in breeched or transversal, placenta previa, or gestational diabetes).
Considered major surgery, a cesarean involves an incision of about 10 to 12 centimeters through seven layers of skin to manually remove the baby from the uterus. Therefore, following post-cesarean care instructions diligently is crucial.
While a c-section can be scheduled in advance, it’s not necessary. In fact, even in cases where a cesarean is genuinely indicated, it’s recommended to wait for the mother to go into labor, allowing the baby to experience contractions aiding in fluid expulsion from the lungs.
The stages of cesarean birth include admission, anesthesia, incision, and layer suturing.
Vaginal Birth (Normal Birth)
Commonly referred to as “normal birth,” vaginal birth encompasses all types of births except cesarean: natural birth, water birth, Leboyer birth, lotus birth, squatting birth, etc.
What sets one type of normal birth apart from another is the assistance provided to the birthing woman and the baby; we’ll explore this further in the next sections.
The stages of normal birth include pre-birth or latent phase (read here about prodromes), labor, birth, and postpartum. Recovery tends to be faster than with cesarean birth, and, in general, the risks are lower.
Natural Birth
Natural birth is a vaginal birth that occurs spontaneously and without medical interventions (e.g., artificial rupture of membranes, induction of labor, episiotomy, or manual exams) and without medications (e.g., analgesia, anesthesia, or synthetic oxytocin).
While it avoids medical interventions, natural birth may involve natural techniques to influence labor progress and aid in pain relief. Techniques such as foot baths or cinnamon tea to stimulate contractions or massages, compresses, and the rebozo technique for pain relief.
Being a type of normal birth, the stages are the same. Recovery tends to be faster, and the advantages for both mother and baby are greater compared to cesarean birth.
Humanized Birth
Humanized birth is built on three pillars: the woman’s protagonism (including access to quality information and informed consent), respectful assistance, and updated scientific evidence.
Ideally, humanized birth shouldn’t be labeled a “type of birth” but rather the standard.
However, the concept of “humanized birth” emerges in contrast to what’s called “normal birth” in hospitals, often involving obstetric violence against women. Humanized birth prioritizes the latest scientific evidence and can occur at home, in the hospital, or at a birthing center.
It may involve medical interventions if they are genuinely indicated for the well-being of the mother and baby, or it may involve no intervention at all. What truly matters is respecting the informed choice of the woman and ensuring decisions and procedures are based on scientific evidence.
Home Birth
Home birth is a vaginal birth that takes place at home. It can only be a normal and/or natural birth, as cesareans must be performed in surgical centers, and medical interventions (such as anesthesia or the application of saline and oxytocin) can only occur in the hospital.
Home births are attended not by obstetric doctors but by obstetric nurses, usually accompanied by other professionals (such as neonatal nurses, physiotherapists, doulas, and/or pediatricians). The team configuration can vary widely, usually composed of 2 to 5 professionals.
Personally, I had a home birth myself when I was pregnant, and also assisted around 15 different women in their home births, and they are my favorite for many, many, many uncountable reasos.
Leboyer Birth
Frédérik Leboyer, a French obstetrician, documented and brought the art of Shantala, an Indian baby massage technique, to the West. Leboyer emphasized the need for a gentle birth and, more importantly, viewing birth from the baby’s perspective.
What’s unique about viewing birth from the baby’s perspective?
Leboyer reminds us that the baby, still in the womb, is in a dark, cozy, protected environment, in direct contact with the mother’s flesh. While we often think of the baby as just kicking in the belly and coming alive after birth, Leboyer points out that the baby is live and already conscious of his/her sensations when going through a full-term birth.
Keeping this in mind, Leboyer suggests a birth with subdued lighting and in a silent environment so that the baby experiences a smooth transition from the uterus to the “world outside.” The umbilical cord should only be cut after it stops pulsating, and the baby should be immediately placed on the mother’s lap, whenever possible, or the father’s. Touch, smell, hearing, and feeling are all taken into account in this transition.

Water Birth
Water birth is a vaginal birth that takes place in the water, ideally in a bathtub or plastic pool (as it’s recommended that the water be heated to 36º to 37º C). However, some women opt to give birth in a river or lake.
The primary advantage of water birth is undoubtedly pain relief and the physical and emotional relaxation that the environment can provide to the birthing woman, ultimately positively impacting the progress of labor. Although it may seem like a new and modern trend, water birth is actually very old. The difference is that today there are conditions and scientific knowledge to perform it more safely for both mother and baby.
Water birth can be done at the woman’s home or at a birthing center. It has also become increasingly common for maternity wards in American hospitals to offer suites with bathtubs for pregnant women who want to have a water birth. However, just like home births, this type of birth is only recommended for low-risk pregnancies.
Lotus Birth
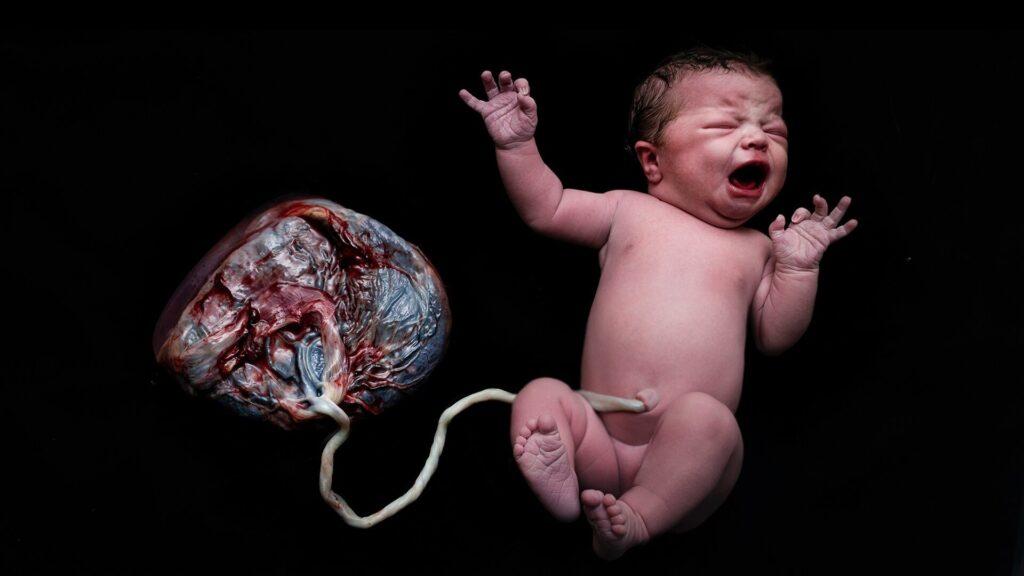
Lotus birth is not exactly a type of childbirth, as the main point here is the baby. That said, lotus birth is vaginal birth that refuses any external intervention not only at the time of birth but also after birth. That is, the placenta must be allowed to be expelled naturally and spontaneously by the body…
And, the key point is not to cut the baby’s umbilical cord, waiting for it to dehydrate and fall off on its own.
Generally, those who opt for a “lotus birth” keep the placenta attached to the already-born baby through the umbilical cord and place it in a basket or pot, where the placenta is “cared for” with salts and plants to avoid a bad smell and rotting. Some babies stay connected to the placenta for 4 to 6 days until the cord falls off.
⚠️ There is no scientific evidence proving the benefits of this practice, and there are risks associated with infection and sepsis development for the baby if organic material contracts any bacteria and transmits it to the newborn.
Normal Birth vs Natural Birth: What are the differences?
Normal birth is any birth that occurs vaginally, with the possibility of medical interventions or medication use. Natural birth is a vaginal birth that occurs without medical intervention (such as episiotomies or forceps) or medication (such as anesthesia and oxytocin). However, it may include natural pain relief techniques.
Natural Birth vs Humanized Birth: What are the differences?
The difference lies in the care. Natural birth is a birth without interventions but can still involve episodes of disrespect for the autonomy of the birthing woman (such as psychological manipulation, moral harassment, blackmail, etc.). Humanized birth is a birth that respects the autonomy and protagonism of the woman and is based on scientific evidence.
Therefore, there may be medical and medication interventions in humanized birth, as long as it is an informed choice of the woman and the procedure is the most appropriate based on science for that situation.
Is it possible to have a normal delivery after a c-section?
Yes, it is entirely possible to have a normal birth after a cesarean. Having a previous c-section is not a risk factor or a real indication for yet another cesarean, according to Oswaldo Cruz Foundation (Fiocruz) – Brazilian organization under the Ministry of Health, the most prominent institution of science and technology in health in Latin America.
Commonly called VBAC (Vaginal Birth After Cesarean), the only requirement is that conditions are favorable.
Usually, the possibility of uterine rupture is used as an argument to dissuade women who have had a previous cesarean from opting for a normal birth.
However, the probability of uterine rupture occurring in a woman who has had a previous cesarean is 0.5% to 1%, and, as Fiocruz points out, this is not something that happens suddenly. Signs can be perceived during labor, allowing and requiring medical intervention before it occurs.
Does the type of delivery or childbirth affect breastfeeding?
Yes, the type of birth can influence breastfeeding. Research shows that breastfeeding in the first hour of life is more common among women who had normal birth (64%) than among those who had a c-section (36%). And it makes perfect sense: after an abdominal cut, breastfeeding may require difficult and uncomfortable logistics for the mother.
In addition to the physical issue of the cut and recovery, hormones also play a significant role. Normal birth releases a load of hormones, called the “love cocktail,” which stimulates milk production and facilitates breastfeeding.
This does not mean that women who had a cesarean will not be able to breastfeed, but they may need a little more patience, stimulation, and support in this process, and they may resort, if necessary, to the help of a Lactation Consultant.
Share this article to spread the word of humanized birth for women and babies!
As we conclude this exploration of childbirth types and possibilities, we hope you’ve gained valuable insights into the diverse ways new life enters the world. Share this knowledge with others and continue your journey by discovering more articles on our blog. Your support helps create a community of informed women ready to embrace the wonders of childbirth!

High-Risk Pregnancy: A Complete Guide For Expecting Mothers | Villa Mater
January 7, 2024 at 7:03 pm[…] is possible for women with high-risk pregnancies to have a normal delivery, but it depends on the specific risk factors involved and the assessment by your doctor. In some […]