Breastfeeding is going smoothly, latch is correct, but suddenly… swelling, redness, engorgement. Mastitis! What now? In this article, we’ll explain what mastitis is, its causes, treatments, and how to relieve the discomfort from this painful inflammation so you can finally get rid of it! Find out!

What is Mastitis?
Mastitis is a breast infection that can occur at any time during breastfeeding. Typically, a lactating woman develops mastitis when bacteria enter the breast tissue through crack nipples or due to milk accumulation in the mammary ducts (clogged breasts or engorgiment).
Types of Mastitis
There are many types of mastitis. Each type is classified by cause or clinical characteristics. Some common types include:
Infectious Mastitis
Caused by a bacterial infection in the breast, usually associated with breastfeeding. It is characterized by breast pain, redness, and swelling, often accompanied by symptoms like fever, chills, and general discomfort.
Periductal Mastitis
Inflammation of the mammary ducts, usually caused by bacterial infection. More common in non-breastfeeding women, periductal mastitis is characterized by pain and redness around the nipple, sometimes accompanied by pus or blood discharge.
Granulomatous Mastitis
A rare type with inflammatory nodules in the breast. More common in young women, it may result from bacterial or fungal infection.
Non-infectious Mastitis
Breast inflammation not caused by an infection. It may result from breast trauma, allergies, autoimmune inflammation, or hormonal contraceptive use.
Mastitis due to untreated Breast Engorgement
Occurs when mammary ducts are obstructed due to milk or fluid accumulation (often referred as “clogged breasts”), leading to breast inflammation and pain.
Clogged Ducts vs Mastitis: are they the same?
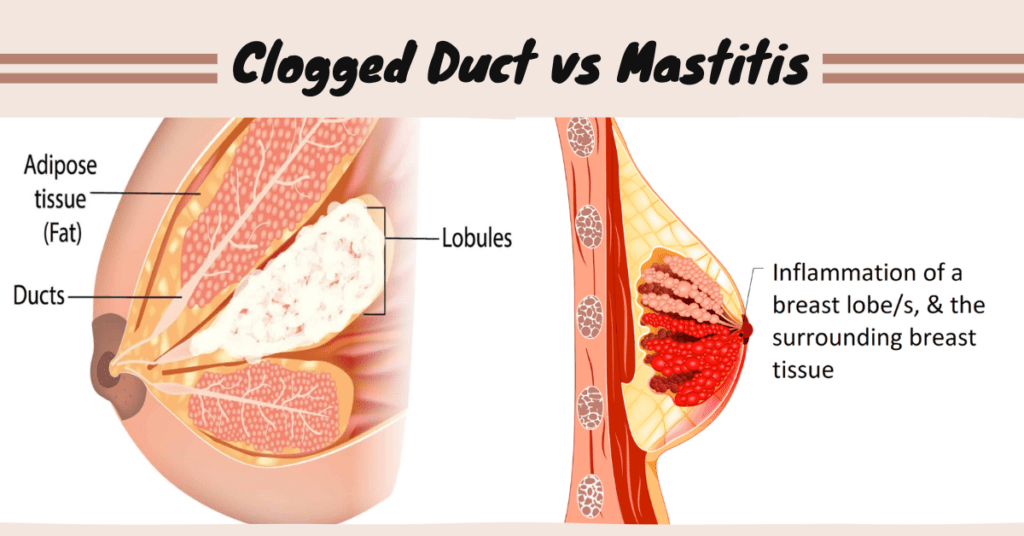
Breast engorgement and mastitis are distinct conditions but may be related.
Breast engorgement, commonly known as “clogged milk” or “clogged breasts” occurs when there is an excessive build-up of milk in the breasts, causing a sensation of heaviness, hardening, and discomfort. Engorgement can be identified not only by discomfort but also by visible nodules, hardened areas in the breast, which are the obstructed ducts.
Doulas and nurses often advise new mothers that babies should empty one breast entirely before offering the other. When a baby doesn’t consume all the milk or when a mother produces more than the baby can drink, milk may become “trapped” in the ducts, accumulating after each feeding, leading to engorgement.
On the other hand, mastitis is an inflammation of the breast, usually caused by bacterial infection. Mastitis may occur when untreated breast engorgement is present or when bacteria enter the breast through a cracked or wounded nipple.
While breast engorgement can lead to mastitis, not every instance of engorgement becomes an infection. This underscores the importance of treating breast engorgement promptly to minimize the risk of developing mastitis.
How to Tell If You Have Mastitis?
If you’re breastfeeding, you may notice that milk isn’t flowing easily from the affected breast. Additionally, you might observe that your milk looks different or has an unusual odor.
Symptoms of Mastitis
Recognizing symptoms can help identify whether you’re developing mastitis or just experiencing breast engorgement. Some common mastitis symptoms include:
- Pain in the inflamed breast;
- Swelling and redness;
- Heat and tenderness in the breast;
- Burning or itching sensation in the nipple;
- High fever (usually above 38.5°C) and chills;
- Fatigue and general malaise;
- Loss of appetite;
- Nausea and vomiting;
- Appearance of lump(s) in the breast;
- Presence of pus or blood from the nipple (rare).
How to Treat Mastitis?
Mastitis treatment typically involves a combination of precautions you should take at home additionally to medications prescribed by a doctor. While there are precautions you can take to alleviate discomfort and speed up the recovery process, medical treatment is essential for resolving the infection entirely.
Medical Treatment
- Use of pain relievers for pain: Consult with a doctor to determine which pain relievers are compatible with breastfeeding.
- Antibiotics: If the infection is bacterial, antibiotics may be necessary to treat mastitis. It’s crucial to follow the prescribed therapy correctly to eliminate the infection; otherwise, mastitis could evolve into a more complex issue.
- Rest whenever possible: Get plenty of rest: If you have a support system, rely on the help of the father, friends, or family to ensure adequate sleep. Avoid overloading the body to accelerate the healing process;
- Use a pump to express milk if the baby doesn’t empty the breast: If you produce more milk than the baby can drink, it’s essential to manually express milk or use a pump to prevent milk from getting trapped in the lactiferous ducts, potentially worsening inflammation. Due to mastitis pain, many women tend to stop breastfeeding to avoid the discomfort. However, continuing to breastfeed can help alleviate breast congestion and prevent worsening mastitis;
- Apply hot and cold compresses: Use hot compresses to alleviate pain and inflammation and cold compresses to help reduce swelling;
- Increase fluid intake to stay hydrated: Drink plenty of water to keep the body hydrated. If you tend to forget to drink water throughout the day, keep a water bottle near where you usually breastfeed or set alarms on your phone as reminders to drink water every hour to maintain your body’s hydration;
- Breast care: Keep the breast with mastitis clean and dry, and wear a comfortable, supportive nursing bra. Avoid bras with underwire and tight-fitting clothing.
What to AVOID if you have a Mastitis
Stop breastfeeding
Continuing to breastfeed is crucial to empty the breast and prevent the infection from worsening, offering almost immediate relief from pain. Frequent breaks in breastfeeding can lead to increased milk accumulation in the breasts, often worsening mastitis and increasing discomfort.
Wearing tight bras
Wearing tight bras can exacerbate swelling and breast pain. Opt for comfortable nursing bras that provide proper support. Hear me out, I had a mastitis after 2 years of on-demand breastfeeding, why? Tight bras. I wouldn’t recommender.
Doing hot compresses excessively
While hot compresses can help alleviate pain and inflammation, excessive heat can worsen the infection. Avoid using hot compresses for more than 20 minutes, and if in doubt, opt for a warm shower, letting the water run over the inflamed breast to relieve pain.
Ignoring symptoms
If you have mastitis, seeking medical treatment immediately is crucial. Ignoring symptoms or delaying treatment can lead to serious complications, making the infection more challenging to treat and potentially interfering permanently with breastfeeding.
Stoping prescribed medications before time
If the doctor has prescribed antibiotics to treat mastitis, it’s essential to take all prescribed medications, even if symptoms improve before the end of treatment. Stopping treatment prematurely can worsen the infection or lead to a recurrence of mastitis, as the cause is not completely eliminated.
Self-medicate
Don’t take any medication without medical guidance, even if it’s a common home remedy. Some remedies may interact with prescribed medications or worsen mastitis symptoms. Always talk to your doctor before taking any medication.
How to Massage Breasts to Relieve Mastitis Pain
Breast massage can help alleviate the pain and discomfort caused by mastitis. To perform the massage, follow these steps:
- Sanitize your hands with soap and water first;
- Warm hands by rubbing them together or wrapping them in a heated cloth;
- Begin by massaging the zone around the breast with gentle circular movements to stimulate milk flow and reduce swelling;
- Place hands in a “C” shape around the breast and make gentle compressing movements, pressing gently downward and backward towards the chest with fingertips;
- Repeat this motion several times across the entire breast;
- If you have a clogged duct or localized pain, place the thumb and forefinger around the affected area and make circular and pressure movements, slowly working towards the nipple. This may help release the blockage and reduce pain;
- Finish the massage with gentle sliding movements on the sides of the breast and chest to help drain any remaining milk and relax the breast.
REMEMBER: breast massage should not be painful. If you experience pain or discomfort during the massage, stop immediately and consult your doctor. Additionally, massage does not replace prescribed medical treatment (such as antibiotics or ointments), so it’s essential to follow your doctor’s guidance to treat the infection correctly.

